obesity
Overweight and obesity are defined as abnormal or excessive fat accumulation that presents a risk to health. A body mass index (BMI) over 25 is considered overweight, and over 30 is obese. The issue has grown to epidemic proportions, with over 4 million people dying each year as a result of being overweight or obese in 2017 according to the global burden of disease.
Overweight and obesity are major risk factors for a number of chronic diseases, including cardiovascular diseases such as heart disease and stroke, which are the leading causes of death worldwide. Being overweight can also lead to diabetes and its associated conditions, including blindness, limb amputations, and the need for dialysis. Rates of diabetes have quadrupled since around the world since 1980. Carrying excess weight can lead to musculoskeletal disorders including osteoarthritis. Obesity is also associated with some cancers, including endometrial, breast, ovarian, prostate, liver, gallbladder, kidney and colon. The risk of these noncommunicable diseases increases even when a person is only slightly overweight and grows more serious as the body mass index (BMI) climbs.
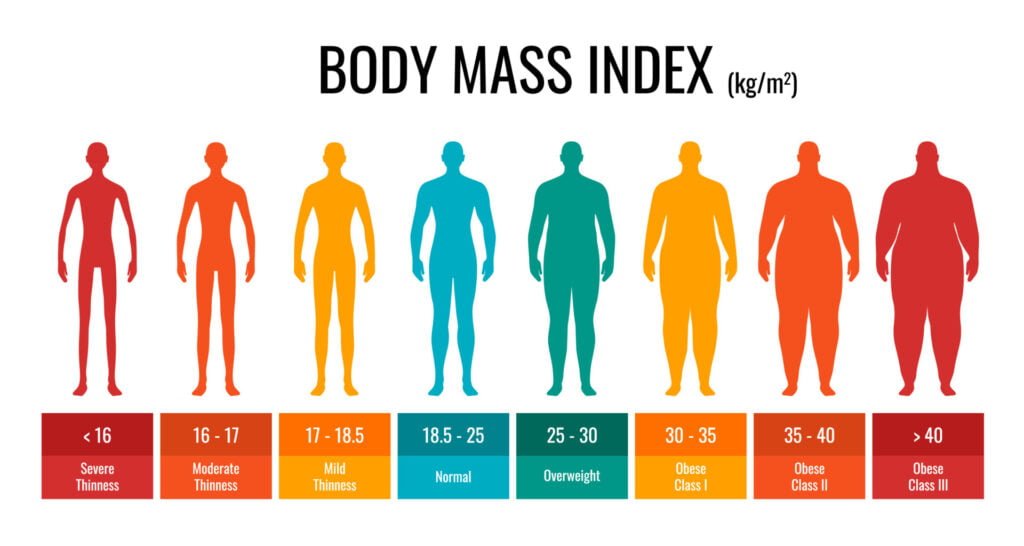
What is Body Mass Index (BMI)?
Body mass index (BMI) is a simple index of weight-for-height that is commonly used to classify overweight and obesity in adults. It is defined as a person’s weight in kilograms divided by the square of his height in meters (kg/m2).
Body mass index, or BMI, is a way to help you figure out if you are at a healthy weight for your height. BMI is a number based on your weight and height. In general, the higher the number, the more body fat a person has. BMI is often used as a screening tool to decide if your weight might be putting you at risk for health problems such as heart disease, diabetes, and cancer.
BMI is used to broadly define different weight groups in adults 20 years old or older.
- Underweight: BMI is less than 18.5
- Normal weight: BMI is 18.5 to 24.9
- Overweight: BMI is 25 to 29.9
- Obese: BMI is 30 or more
Calculate your BMI.
You can also calculate your own BMI. The actual formula to determine BMI uses metric system measurements: weight in kilograms (kg) divided by height in meters, squared (m2).
When using pounds and inches, the formula needs to be altered slightly. Multiply your weight in pounds by 703. Divide that by your height in inches, squared:
BMI = (your weight in pounds x 703) ÷ (your height in inches x your height in inches)
What causes obesity?
The fundamental cause of obesity and overweight is an energy imbalance between calories consumed and calories expended. Globally, there has been:
- an increased intake of energy-dense foods that are high in fat and sugars; and
- an increase in physical inactivity due to the increasingly sedentary nature of many forms of work, changing modes of transportation, and increasing urbanization.
Changes in dietary and physical activity patterns are often the result of environmental and societal changes associated with development and lack of supportive policies in sectors such as health, agriculture, transport, urban planning, environment, food processing, distribution, marketing, and education.
Fact sheet !
Obesity currently affects four out of 10 Americans, according to data from the Centers for Disease Control and Prevention (CDC). While weight and overall health aren’t always connected, obesity is often considered a cause of multiple comorbid and chronic medical conditions, including type 2 diabetes, some forms of cancer and heart disease.
Digging into the statistics about obesity in the U.S. can help paint a picture of why rates continue to climb, as well as what can be done to slow (or even reverse) these trends.
- Obesity is linked to 30% to 53% of new diabetes cases in the U.S. every year, per research in the Journal of the American Heart Association.
- Based on data collected between 2017 and 2020, 41.9% of adults in the U.S. have obesity.
- The same data set suggests 19.7% of adolescents and children in the U.S.—14.7 million individuals— have obesity.
- Worldwide, more than 1 billion people have obesity—650 million adults, 340 million adolescents and 39 million children, according to WHO[.
- The obesity rate in the U.S. continued to climb during the COVID-19 pandemic, increasing by 3% between March 2020 and March 2021.
- Worldwide obesity has nearly tripled since 1975.
- In 2016, more than 1.9 billion adults, 18 years and older, were overweight. Of these over 650 million were obese.
- 39% of adults aged 18 years and over were overweight in 2016, and 13% were obese.
- Most of the world’s population live in countries where overweight and obesity kills more people than underweight.
- 39 million children under the age of 5 were overweight or obese in 2020.
- Over 340 million children and adolescents aged 5-19 were overweight or obese in 2016.
- Obesity is preventable.
Socio-economic & demographic correlation of obesity!
- Four million people die each year as a result of obesity, according to the World Health Organization (WHO).
- The worldwide obesity rate has nearly doubled since 1980.
- The World Obesity Federation predicts that by 2030, one in five women and one in seven men will have obesity.
- Currently, more people have obesity than underweight in every region of the world, with the exception of sub-Saharan Africa and Asia, revealing how it’s a common health problem in both developed and developing countries.
Obesity and America
- Nineteen states have an adult obesity rate that exceeds 35%.
- At 40.3%, West Virginia has the highest obesity rate in the country.
- Washington, D.C. has the lowest obesity rate of 24.7%.
- Obesity rates aren’t worsening in every state. In fact, the obesity rate in California decreased by 2.7% between 2020 and 2021, showing the most significant improvement of any state.
- Meanwhile, other states are witnessing significant increases to their obesity rates. South Dakota’s obesity rate increased by 5.2% from 2020 to 2021.
- According to the 2022 State of Obesity report, Black adults have the highest rate of obesity in the U.S.—49.9%—compared to 45.6% of Hispanic adults, 41.4% of white adults and 16.1% of Asian adults.
- U.S. adults who live in rural areas are more likely to have obesity than U.S. adults living in urban areas, according to the CDC.
Trends in Obesity among Adults and Youth in the United States
Adults
Trends in obesity and severe obesity prevalence among adults ages 20 and over: United States, 1999–2000 through 2017–20187.
1Significant linear trend.
NOTES: Estimates were age adjusted by the direct method to the 2000 U.S. Census population using the age groups 20–39, 40–59, and 60.
SOURCE: National Center for Health Statistics, National Health and Nutrition Examination Survey, 1999–2018. As shown in the figure above
- The prevalence of obesity and severe obesity increased significantly among adult men and women between 1999–2000 and 2017–2018.
Youth
Trends in obesity among children and adolescents ages 2–19 years, by age: United States, 1963–1965 through 2017–2018
NOTE: Obesity is defined as body mass index (BMI) at or above the 95th percentile from the sex-specific BMI-for-age 2000 CDC Growth Charts.
SOURCES: National Center for Health Statistics, National Health Examination Surveys II (ages 6–11) and III (ages 12–17); and National Health and Nutrition Examination Surveys (NHANES) I–III, and NHANES 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2018.
As shown in the above line graph
- The prevalence of obesity among children and adolescents ages 2 to 19 years roughly doubled between 1988–1994 and 2017–2018.
- Among children ages 2 to 5, the prevalence of obesity increased between 1988–1994 and 2003–2004, decreased between 2003–2004 and 2011–2012, and then increased again.
- Among children ages 6 to 11, the prevalence of obesity increased between 1988–1994 and 2003–2004, fluctuated over the next several years, and most recently (2013–2014 to 2017–2018) increased.
- Among adolescents, ages 12 to 19, the prevalence of obesity has increased between 1988–1994 and 2017–2018.
1) Global obesity 2020~2035
3) Country Preparedness by country income group and region
High income regions
High income countries are defined by the World Bank as those with a GNI per capita of US$13,205 or more. In high income countries, childhood obesity levels are similar to those in upper-middle income countries. Although expected to rise over the period 2020-2035, the prevalence of childhood obesity in high income countries is likely to be overtaken by the prevalence in upper-middle income countries. For adults, high income countries show the greatest obesity prevalence levels of any income group, and this continues throughout the period, with obesity prevalence expected to reach 37% of women and 42% of men by 2035. The economic impact was estimated to exceed US$1.3 trillion in 2020, rising to nearly US$2.3 trillion annually by 2035 (at constant 2019 dollars), equivalent to 3% of high income countries’ GDP at the time.
Upper-middle income countries
Countries with a GNI per capita between US$4,256 and USS$13,205 are defined by the World Bank as being upper-middle income. Compared with children and adolescents in lower-middle income countries, those in upper-middle income countries are predicted to experience very high levels of obesity prevalence by 2035, with 31% of girls and 40% of boys living with obesity. Adults are predicted to reach 27% prevalence of obesity by 2035. The economic impact is predicted to exceed an annual US$1.6 trillion (at constant 2019 dollars) by 2035, equivalent to more than 3% of upper-middle income countries’ GDP at the time.
Low income countries
The World Bank defines low income as countries with a gross national income (GNI) per capita of less than
US$1,085 in 2021. Children and adolescents in low income countries are likely to experience a dramatic increase in the prevalence of obesity during the period 2020 to 2035, from 4% to 13% of girls, and from 2% to 6% of boys.
The average prevalence of obesity in adults is expected to double over the period, from 5% to 11% of men, and from 14% to 26% of women. The economic impact of high BMI is predicted to reach US$9billion annually by 2035 (at constant 2019 dollars), equivalent to over 1% of low income countries’ GDP at the time.
Lower-middle income countries
Lower-middle income countries are defined by the World Bank as those with a GNI per capita between US$1,086
and $4,255. In lower-middle income economies, children and adolescents are likely to see a marked increase in the prevalence of obesity during the period 2020 to 2035, from 5% to 14% of girls, and from 6% to 16% of boys. For adults, the prevalence of obesity is expected to nearly double over the period, from 7% to 14% of men, and from 13% to 23% of women. The economic impact of high BMI is predicted to reach US$362 billion annually by 2035 (at constant 2019 dollars), equivalent to over 2% of lower-middle income countries’ GDP at the time.
By country income group and region
Obesity related complications !
People with obesity are more likely to develop a number of potentially serious health problems, including:
- Heart disease and strokes. Obesity makes you more likely to have high blood pressure and unhealthy cholesterol levels, which are risk factors for heart disease and strokes.
- Type 2 diabetes. Obesity can affect the way the body uses insulin to control blood sugar levels. This raises the risk of insulin resistance and diabetes.
- Certain cancers. Obesity may increase the risk of cancer of the uterus, cervix, endometrium, ovary, breast, colon, rectum, esophagus, liver, gallbladder, pancreas, kidney and prostate.
- Digestive problems. Obesity increases the likelihood of developing heartburn, gallbladder disease and liver problems.
- Sleep apnea. People with obesity are more likely to have sleep apnea, a potentially serious disorder in which breathing repeatedly stops and starts during sleep.
- Osteoarthritis. Obesity increases the stress placed on weight-bearing joints. It also promotes inflammation, which includes swelling, pain and a feeling of heat within the body. These factors may lead to complications such as osteoarthritis.
- Fatty liver disease. Obesity increases the risk of fatty liver disease, a condition that happens due to excessive fat deposit in the liver. In some cases, this can lead to serious liver damage, known as liver cirrhosis.
- Severe COVID-19 symptoms. Obesity increases the risk of developing severe symptoms if you become infected with the virus that causes coronavirus disease 2019, known as COVID-19. People who have severe cases of COVID-19 may need treatment in intensive care units or even mechanical assistance to breathe.
Cause and risk factors
Cause
Although there are genetic, behavioral, metabolic and hormonal influences on body weight, obesity occurs when you take in more calories than you burn through typical daily activities and exercise. Your body stores these excess calories as fat.
In the United States, most people’s diets are too high in calories — often from fast food and high-calorie beverages. People with obesity might eat more calories before feeling full, feel hungry sooner, or eat more due to stress or anxiety.
Many people who live in Western countries now have jobs that are much less physically demanding, so they don’t tend to burn as many calories at work. Even daily activities use fewer calories, courtesy of conveniences such as remote controls, escalators, online shopping, and drive-through restaurants and banks.
Risk factors
Family inheritance and influences
The genes you inherit from your parents may affect the amount of body fat you store, and where that fat is distributed. Genetics also may play a role in how efficiently your body converts food into energy, how your body regulates your appetite and how your body burns calories during exercise.
Obesity tends to run in families. That’s not just because of the genes they share. Family members also tend to share similar eating and activity habits.
Lifestyle choices
- Unhealthy diet. A diet that’s high in calories, lacking in fruits and vegetables, full of fast food, and laden with high-calorie beverages and oversized portions contributes to weight gain.
- Liquid calories. People can drink many calories without feeling full, especially calories from alcohol. Other high-calorie beverages, such as sugared soft drinks, can contribute to weight gain.
- Inactivity. If you have an inactive lifestyle, you can easily take in more calories every day than you burn through exercise and routine daily activities. Looking at computer, tablet and phone screens is inactivity. The number of hours spent in front of a screen is highly associated with weight gain.
Certain diseases and medications
In some people, obesity can be traced to a medical cause, such as hypothyroidism, Cushing syndrome, Prader-Willi syndrome and other conditions. Medical problems, such as arthritis, also can lead to decreased activity, which may result in weight gain.
Some medicines can lead to weight gain if you don’t compensate through diet or activity. These medicines include steroids, some antidepressants, anti-seizure medicines, diabetes medicines, antipsychotic medicines and certain beta blockers.
Other factors
Age
Obesity can occur at any age, even in young children. But as you age, hormonal changes and a less active lifestyle increase your risk of obesity. The amount of muscle in your body also tends to decrease with age. Lower muscle mass often leads to a decrease in metabolism. These changes also reduce calorie needs and can make it harder to keep off excess weight. If you don’t consciously control what you eat and become more physically active as you age, you’ll likely gain weight.
Pregnancy
Weight gain is common during pregnancy. Some women find this weight difficult to lose after the baby is born. This weight gain may contribute to the development of obesity in women
Microbiome
The make-up of your gut bacteria is affected by what you eat and may contribute to weight gain or trouble losing weight.
Quitting smoking, Lack of sleep, Stress all contribute in obesity
Treatment of obesity
The goal of obesity treatment is to reach and stay at a healthy weight. This improves overall health and lowers the risk of developing complications related to obesity.
You may need to work with a team of health professionals — including a dietitian, behavioral counselor or an obesity specialist — to help you understand and make changes in your eating and activity habits.
The first treatment goal is usually a modest weight loss — 5% to 10% of your total weight. That means that if you weigh 200 pounds (91 kilograms), you’d need to lose only about 10 to 20 pounds (4.5 to 9 kilograms) for your health to begin to improve. But the more weight you lose, the greater the benefits.
All weight-loss programs require that you change your eating habits and get more active. The treatment methods that are right for you depend on your weight, your overall health and your willingness to participate in a weight-loss plan.
Dietary changes
Reducing calories and practicing healthier eating habits are key to overcoming obesity. Although you may lose weight quickly at first, steady weight loss over the long term is considered the safest way to lose weight. It’s also the best way to keep weight off permanently.
There is no best weight-loss diet. Choose one that includes healthy foods that you feel will work for you. Dietary changes to treat obesity include:
- Cutting calories. The key to weight loss is reducing how many calories you take in. The first step is to review your typical eating and drinking habits. You can see how many calories you usually consume and where you can cut back. You and your health care professional can decide how many calories you need to take in each day to lose weight. A typical amount is 1,200 to 1,500 calories for women and 1,500 to 1,800 for men.
- Feeling full on less. Some foods — such as desserts, candies, fats and processed foods — contain a lot of calories for a small portion. In contrast, fruits and vegetables provide a larger portion size with fewer calories. By eating larger portions of foods that have fewer calories, you can reduce hunger pangs and take in fewer calories. You also may feel better about your meal, which contributes to how satisfied you feel overall.
- Making healthier choices. To make your overall diet healthier, eat more plant-based foods. These include fruits, vegetables and whole grains. Also emphasize lean sources of protein — such as beans, lentils and soy — and lean meats. If you like fish, try to include fish twice a week. Limit salt and added sugar. Eat small amounts of fats, and make sure they come from heart-healthy sources, such as olive, canola and nut oils.
- Restricting certain foods. Certain diets limit the amount of a particular food group, such as high-carbohydrate or full-fat foods. Ask your health care professional which diet plans are effective and which might be helpful for you. Drinking sugar-sweetened beverages is a sure way to consume more calories than you intended. Limiting these drinks or eliminating them altogether is a good place to start cutting calories.
- Meal replacements. These plans suggest replacing one or two meals each day with their products — such as low-calorie shakes or meal bars — and eating healthy snacks. Then you have a healthy, balanced third meal that’s low in fat and calories. In the short term, this type of diet can help you lose weight. But these diets likely won’t teach you how to change your overall lifestyle. So you may have to stay on the diet if you want to keep your weight off.
Similarly, you may lose weight on a crash diet, but you’re likely to regain it when you stop the diet. To lose weight — and keep it off — you must adopt healthy-eating habits that you can maintain over time.
Exercise and activity
Getting more physical activity or exercise is an essential part of obesity treatment:
- Exercise. People with obesity need to get at least 150 minutes a week of moderate-intensity physical activity. This can help prevent further weight gain or maintain the loss of a modest amount of weight. You’ll probably need to gradually increase the amount you exercise as your endurance and fitness improve.
- Keep moving. Even though regular aerobic exercise is the most efficient way to burn calories and shed excess weight, any extra movement helps burn calories. For example, park farther from store entrances and take the stairs instead of the elevator. A pedometer can track how many steps you take over the course of a day. Many people try to reach 10,000 steps every day. Gradually increase the number of steps you take daily to reach your goal.
Weight-loss medicines
Weight-loss medicines are meant to be used along with diet, exercise and behavior changes, not instead of them. Before selecting a medication for you, your health care professional will consider your health history, as well as possible side effects.
The most commonly used medications approved by the U.S. Food and Drug Administration (FDA) for the treatment of obesity include:
- Bupropion-naltrexone (Contrave).
- Liraglutide (Saxenda).
- Orlistat (Alli, Xenical).
- Phentermine-topiramate (Qsymia).
- Semaglutide (Ozempic, Rybelsus, Wegovy).
Weight-loss medicines may not work for everyone, and the effects may wane over time. When you stop taking a weight-loss medicine, you may regain much or all of the weight you lost.
Other methods are .
Behavior changes
Endoscopic procedures for weight loss
Weight-loss surgery
Hydrogels
Gastric aspirate
Notice
“Obesity is the biggest disease of mankind – bigger than even cancer. Your self-confidence is low and you become mentally sick.”
— Vital organisation